Sleep disturbances are among the most common complaints in patients after completing chemotherapy. Research shows that approximately 30–50% of individuals who have undergone cancer treatment report some degree of insomnia, frequent nocturnal awakenings, sleep anxiety, or non-restorative sleep.
These disturbances arise from various factors, including hormonal changes, chemotherapy-related effects on the nervous system, inflammation, anxiety, and reduced physical activity levels.
Scientific evidence demonstrates that light, targeted exercises can significantly improve sleep quality in patients after chemotherapy—without placing unnecessary stress on the recovering body.
This article, based on scientific data, introduces exercise practices shown to have the greatest impact on sleep improvement after chemotherapy.
1. Why Are Sleep Disturbances Common After Chemotherapy?
Sleep is a complex biological process regulated by hormonal, neurological, and immunological pathways. Chemotherapy, while one of the most effective cancer treatments, can temporarily disrupt these pathways.
Many patients therefore experience a period of sleep irregularity after treatment. This period does not necessarily indicate a lasting problem in the body; rather, it reflects a temporary phase of the body’s natural re-regulation process.
Clinical studies attribute sleep disturbances mainly to two groups of factors:
Physical Factors
- Hormonal fluctuations
Changes in cortisol, melatonin, and thermoregulatory hormones can destabilize the sleep–wake cycle. - Inflammation caused by medications
Chemotherapy may trigger inflammatory responses that heighten nervous system sensitivity. - Diffuse muscle or bone pain
Such discomfort decreases sleep depth and increases nighttime awakenings. - Physical symptoms such as nausea, hot flashes, or palpitations
These can make the process of falling asleep more difficult. - Medications taken alongside chemotherapy
For example, steroids alter energy levels and circadian rhythms.
Psychological Factors
- Anxiety related to the treatment process
Keeps the mind alert and prevents the down-regulation of the nervous system. - Worries about the future, follow-up scans, or recurrence
One of the most common drivers of sleep disturbance after treatment. - Daily life stressors and changes in routine
Stress elevates cortisol and interferes with relaxation. - Disrupted sleep routines
Irregular sleep–wake schedules during treatment may persist afterward.
This combination of factors means the body often needs targeted interventions to regain sleep balance.
Among the most reliable and effective interventions are light, controlled physical exercises that gradually help reset the sleep–wake rhythm.

2. How Does Exercise Improve Sleep?
Clinical studies and systematic reviews, including reports published by the National Cancer Institute (NCI), have shown that exercise can improve the following outcomes:
- Regulate the circadian rhythm
Regular physical activity normalizes melatonin and cortisol secretion. - Reduce stress and anxiety
Exercise lowers stress hormone levels and induces mental relaxation. - Reduce cancer-related fatigue
Studies show exercise directly decreases chronic fatigue and prepares the body for better sleep. - Increase endorphins
Light activity promotes a sense of calm, balance, and well-being.
These combined effects significantly enhance sleep quality—and importantly, even very light exercises can be effective.
For this reason, specialists recommend incorporating various forms of exercise after treatment to support and improve sleep quality. Understanding the close relationship between physical movement and mental well-being helps explain why gentle exercise can significantly improve sleep after chemotherapy.
3. What Types of Exercise Are Most Effective for Improving Sleep After Chemotherapy?
The best exercises for improving sleep after chemotherapy are those that help relax the body, reduce tension, and prepare the mind for restful sleep. According to research, five types of exercises have the greatest impact on sleep quality in patients:
1) Light Walking
Nothing is as consistently effective as this simple, low-intensity activity. Walking is the easiest and most effective way to calm the nervous system and reduce post-chemotherapy insomnia.
How to do it:
- Walk gently for 10–15 minutes
On a flat, smooth path at a pace that does not disrupt your breathing. - Gradually increase duration
After 1–2 weeks, increase to 20–30 minutes.
Frequency: 3–4 days per week
Best time: Late afternoon or before sunset—when body temperature naturally begins to fall.
Effect: Regulates circadian rhythm, reduces bodily tension, improves sleep onset.
2) Gentle Stretching
These gentle stretches relieve muscle tension, calm the nervous system, and are considered clinically safe for people after chemotherapy. The movements below are short, simple, and non-strenuous.
- Neck stretch
Gently tilt the head to one side until a mild stretch is felt. Hold for 15–20 seconds, then repeat on the other side.
Benefit: Reduces shoulder and neck tension and promotes early relaxation before bedtime. - Chest stretch (against a wall)
Stand next to a wall and place your hand on it. Slowly rotate your torso away from the wall until you feel a gentle stretch across the front of the chest. Hold for about 15 seconds.
Benefit: Helpful for people who experience tightness or stiffness in the chest and shoulders after chemotherapy. - Gentle Cat–Cow movement
Come onto hands and knees. Slowly round the back (cat), then lower it and open the chest (cow). Repeat 8–10 times with slow, controlled breathing.
Benefit: Soothes the spine, regulates breathing, and prepares the body for sleep.

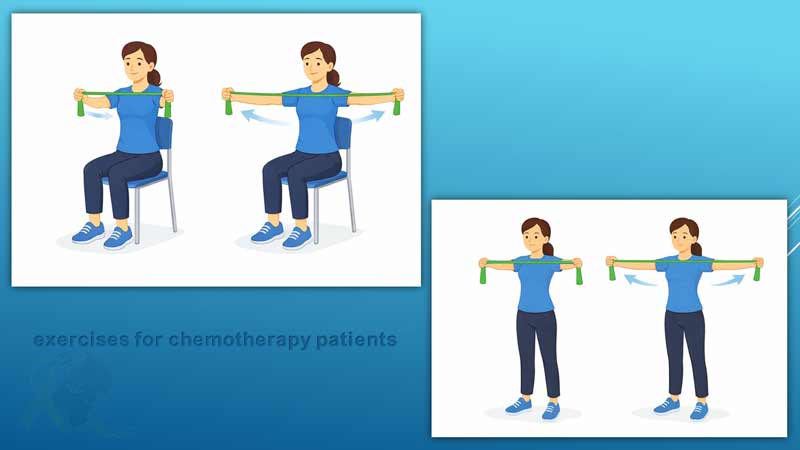
3) Very Light Resistance Training
These exercises improve sleep quality by increasing muscle strength and reducing overall fatigue. They can be performed using resistance bands, 0.5-kg dumbbells, or even just your own body weight. The movements below are short, safe, and low-intensity:
- Chest opener with a resistance band
Hold the band with both hands and gently open your arms to the sides.
Perform 10 repetitions.
Benefit: Helps reduce tightness in the shoulders and chest, and improves breathing. - Light shoulder raise with small dumbbells
Lift 0.5-kg dumbbells with straight arms up to shoulder height.
Perform 8–10 repetitions.
Benefit: Strengthens the shoulders without adding strain. - Mini squat with support
While holding onto a wall or chair, bend your knees slightly and return to standing.
Perform 6–8 repetitions.
Benefit: Increases leg strength and helps reduce daily fatigue.
4) Restorative Yoga
Restorative yoga is one of the most effective mind–body practices for improving sleep in cancer survivors.
It helps activate the parasympathetic nervous system.
The following poses are short, safe, and low-pressure:
- Child’s Pose
Kneel down, slowly lower your torso forward, and extend your arms in front of you.
Hold for 20–30 seconds.
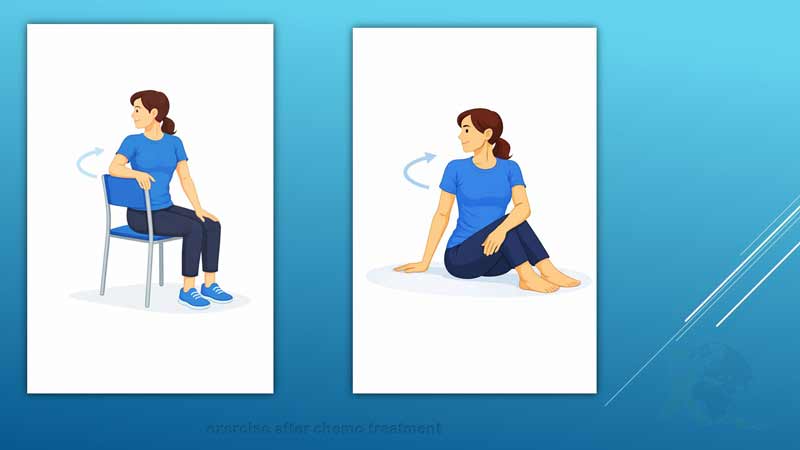
Benefit: Creates a sense of relaxation and reduces lower-back tension. - Seated Spinal Twist
Sit comfortably and gently rotate your torso to the right, then to the left.
Hold for 15 seconds on each side.
Benefit: Relieves back tightness and helps open the chest. - Seated Butterfly Stretch
Bring the soles of your feet together, let your knees fall to the sides, and lean slightly forward.
Hold for 20 seconds.
Benefit: Relaxes the pelvic area and reduces nervous tension.
5) Relaxation and Breathing Exercises
These exercises include diaphragmatic breathing, progressive muscle relaxation, body scan, and relaxation imagery. All of them help the body shift from a state of “alertness and stress” to “deep relaxation.”
By lowering heart rate, regulating breathing, and reducing muscle tension, these techniques create the conditions needed for falling asleep and decreasing nighttime awakenings.They can easily be incorporated into the nightly routine.

4. Practical 4–8 Week Exercise Plan
(Designed for three different energy levels)
This post-chemotherapy exercise program is tailored to fatigue, physical capacity, and individual daily condition.
Level 0 — For days when the body feels very weak
• 5 minutes of walking indoors or in the yard
• 3 minutes of diaphragmatic breathing
• 2 gentle stretches, such as:
– Neck stretch
– Shoulder stretch
This level is for days with very low energy. Even this small amount makes a difference.
Level 1 — Moderate energy level
• 10–15 minutes of walking
• 5 minutes of gentle stretching
• 5 minutes of breathing exercises
Best time to exercise:
Morning or afternoon
(not close to bedtime)
Level 2 — Higher readiness
• 20–30 minutes of walking
• 5 minutes of very light resistance training
• 5 minutes of gentle yoga
• 3 minutes of relaxation
This level is appropriate when the body allows for gradual progress.
5. Scientific Sleep Routine for Improving Post-Chemotherapy Insomnia (Sleep Hygiene)
Scientific evidence shows that a combination of behavioral and environmental strategies can help restore the body’s sleep system and reduce insomnia.
This collection of habits—known as sleep hygiene—is one of the main recommendations provided by cancer-care specialists, because it improves sleep onset and reduces nighttime awakenings without the need for medication.
In this section, we review the key sleep-hygiene principles specifically adapted for patients after chemotherapy.
✔ Go to bed and wake up at the same time every day
Even on weekends.
✔ Keep daytime naps under 30 minutes
And avoid napping close to the evening.
✔ Keep the bedroom dark, cool, and free of electronic devices
Blue light = melatonin’s enemy.
✔ Avoid eating before bedtime
Especially heavy, spicy, sugary, or acidic foods.
✔ If you cannot fall asleep after 20 minutes
Get out of bed and do a quiet, calming activity in another room.
✔ Avoid exercising if less than 3 hours remain before bedtime
The body is still warm and physiologically active.
Following sleep-hygiene principles—even in their simplest form—helps the body return to its natural state of rest and relaxation. These small but powerful habits are among the most reliable ways to reduce post-chemotherapy insomnia and support the body’s healing process.
6. Combining Exercise with Mind–Body Relaxation: The Best Approach for Deep Sleep
Research shows that combining physical activity with mental relaxation creates the most effective results for improving sleep in patients after chemotherapy.
Here is a simple 10-minute routine to perform at the end of the day:
✔ 1 minute of deep breathing
Inhale for 4 seconds → hold for 2 seconds → exhale for 6 seconds
✔ 4 minutes of gentle stretching
Neck stretch, shoulder stretch, chest stretch, and lower-back stretch
✔ 5 minutes of relaxation or body scan
Move your attention gradually from the toes up to the top of the head.
This short routine acts like a calming bridge between day and night, helping the body transition into deeper sleep.
7. Safety Guidelines for Exercising After Treatment
These precautions are essential for your safety:
- If you experience fever, dizziness, shortness of breath, chest pain, or unusual fatigue → stop exercising immediately.
- If you have high blood pressure or any cardiac conditions → consult your doctor before exercising.
- Your body may feel weaker for several days after a chemotherapy infusion — this is normal.
- If you have neuropathy, use supportive footwear and exercise on soft, stable surfaces.
- Avoid intense, fast, or heavy movements.
- Stay well hydrated. Dehydration can disrupt sleep.
Exercise should support your recovery — not place stress on your body.
8. Final Message from Care & Healing
Sleep disturbances after chemotherapy are common, yet highly manageable. Research clearly shows that the body has an impressive ability to restore itself and re-regulate essential functions after cancer treatment—provided it receives the right support and conditions. Regular physical activity, even in its simplest forms, is one of the most effective tools in this process. It can stabilize sleep rhythms, reduce stress, and gently bring a sense of calm back to the body—without the need for medication.
Clinical studies—including trials conducted on breast cancer patients—indicate that combining proper sleep hygiene with light physical activity often leads to initial improvements within the first 2 to 4 weeks. More stable and reliable progress typically appears within 6 to 10 weeks, and many survivors notice consistent, measurable changes in their sleep quality within 8 to 12 weeks. This timeline is completely natural, as the body needs time to rebuild its circadian rhythm, restore hormonal balance, and regulate the nervous system.
After treatment, your body needs time, support, and predictable rhythms. These gentle exercises are a safe and effective way to restore calm, improve sleep quality, and support your recovery journey. With steady, consistent practice, better sleep becomes not just a hope—but an expected outcome.

I can’t sleep after chemotherapy and wake up multiple times at night. Are there any safe exercises that can help me sleep better?
It’s normal for cancer survivors to have trouble sleeping after treatment. Studies show that exercising after treatment, even with gentle walking, stretching, or exercises to improve sleep after chemotherapy, can help restore your sleep rhythm. Incorporating sleep improvement exercises for breast cancer survivors gradually reduces nighttime awakenings. Always start slowly and consult your doctor if problems persist.
I’ve been struggling to sleep after chemotherapy. Are there any solutions? I’ve heard about best sleeping pills for cancer patients, but I’m not sure if I should use them.
Many cancer survivors wonder about sleeping pills, but research shows that gentle exercises, stretching, yoga, and good sleep hygiene can often improve sleep naturally without medication. If sleep problems persist, you should consult your doctor before considering any pills. Combining light physical activity with relaxation techniques is usually a safe and effective approach for improving post-chemotherapy sleep.
I’m still undergoing chemo infusions and I’m worried about my sleep. Is it safe to do exercise during chemotherapy infusion? I don’t want to push myself too much, but I feel some movement might help me not feel so restless during the day.
During infusion, only very light exercises like gentle stretching of hands, neck, or shoulders are safe and can help reduce tension. While exercise during chemotherapy infusion won’t replace post-treatment routines, it can help your body stay lightly active and improve alertness, which may indirectly benefit sleep after chemotherapy.
Lately, I’ve noticed I’m extremely drowsy and often nap during the day. Does chemotherapy make you sleep all the time? I want to stay active but still get proper sleep after chemo. Can light exercises after chemotherapy help regulate my energy levels and improve nighttime rest?
Yes, feeling excessively sleepy after treatment is common, but gentle activity can help. Short walks, light stretching, or restorative yoga as exercises after chemotherapy can reduce daytime drowsiness, balance energy, and support better sleep after chemo. Your body is gradually re-regulating, and these small steps can make a big difference.
Why can’t I sleep after chemotherapy? I try to rest, but my sleep is still poor. I wake up feeling exhausted, and it’s affecting my mood and daily energy. I don’t know how to get back to a normal sleep routine.
Difficulty sleeping after chemotherapy is common, and it’s often linked to changes in your circadian rhythm and nervous system. Exercising when recovering from treatment, even in very gentle forms like light stretching, short walks, or restorative yoga, can help your body relax and regulate sleep patterns. Unlike medications, these exercises to improve sleep after chemotherapy also reduce stress and fatigue gradually. Pairing them with calming bedtime routines and proper sleep hygiene can make sleep more restorative.